The challenge
In mid and west Wales Hywel Dda University Health Board has an ageing population living across a large and largely rural geographic area, which presents additional challenges to the effective delivery of healthcare services. The pandemic also had a significant impact on elective waiting lists, which in turn adversely affected patients’ physical and psychological wellbeing. How has Hywel Dda UHB worked with Llesiant Delta Wellbeing and Tunstall Healthcare to introduce a virtual prehabilitation model supported by remote patient monitoring (RPM) to help address these challenges?
What we did
Using Welsh Government Out-Patient Transformation funding, stakeholders worked together to plan and implement:
- Governance, reporting and evaluation arrangements
- Staff training
- Prehab equipment bundle, including patient information leaflets
- Decision tree for clinical escalation
- MDT assessment template
The healthcare system is treating larger numbers of patients with fewer or more limited resources. With telehealth (RPM) we can monitor more people than with conventional methods, due to decreased travel time/costs and consultation times. It helps our patients to stay well by improving their self management and helps them avoid or deal better with exacerbations.
Marilize du Preez, Improvement and Transformation Lead, Hywel Dda University Health Board
Virtual first delivery model
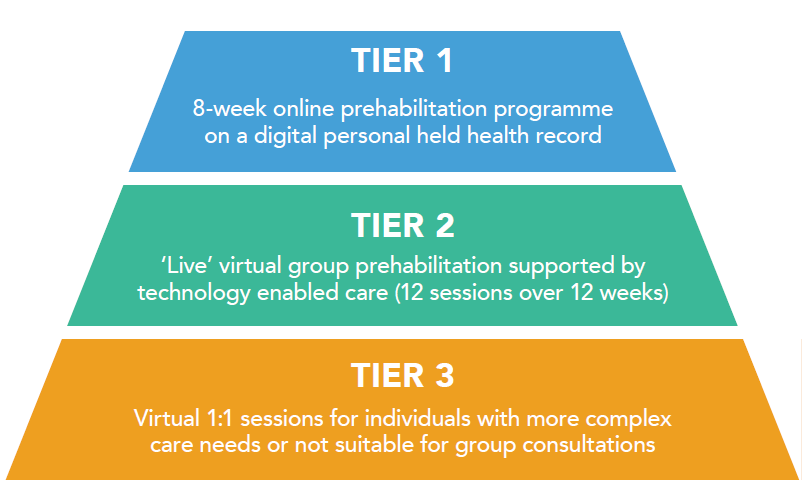
The service was offered to priority patients/ longest waits based on outcome of individual assessment, clinical need and shared decision making, and was delivered in three tiers:
Patients were assessed and those suitable set up on the Tunstall RPM platform (Tier 2). The Hywel Dda UHB clinical team established parameters for each patient which would raise an alert on the ICP triagemanager software if breached. Delta Wellbeing then delivered the Prehab technology and supporting information, and gave patients step by step advice on how to access and use their prehabilitation plan and input data from their devices, e.g. blood pressure monitor, thermometer, weighing scales using the myMobile app.
Patients can use their own smart devices to use the app, although 21 patients who had previously never used technology before were provided with tablets and successfully supported to start using digital platforms.
Each patient takes vital signs readings twice a week, which are uploaded to the myMobile app via Bluetooth connectivity. This negates the need for patients to enter their readings manually.
They also answer a series of questions that relate to their general health. This helps the clinical team to identify any subtle changes to the patients’ health and act to mitigate these changes. This information is then collected by the triagemanager software, where it will alert clinicians if required so they can contact the patient. Clinicians can review the readings remotely at any time, and they are stored on the patient file so can be exported to the patient’s clinical notes. Clinical staff can also use the app to message patients, and patients attend virtual group prehabilitation sessions. Additional weekly exercise videos and resources are also available on the app.
Once patients have completed the programme, the equipment is collected, cleaned, checked and stored by Delta Wellbeing, ready to be re-used for the next patient cohort.

Results
Currently (May 2023) 164 patients have used the service, with both patients and staff reporting positive experiences. The resulting evidence indicates RPM supported by clinical team leads to behavioural change with improved physical and psychological outcomes, including:
- High programme completion rate (less than 9% drop out rate)
- 64% of patients lost weight (average loss 2.8 kg)
- 17% of patients lost more than 4kg
- Improved Oxford scores*
- Increased level of physical activity per week
- Improved health management (blood pressure)
- Improved access to the relevant health professional at the right time
- Reduction in length of hospital stay at the point of surgery**
Find out more about Tunstall's Remote Patient Monitoring solution
* The Oxford Knee Score is a patient reported outcome measure that consists of 12 questions about an individual’s level of function, activities of daily living and how they have been affected by pain over the preceding four weeks.
** Compared to Getting It Right First Time (GIRFT) data - a national programme designed to improve the treatment and care of patients through in-depth review of services, benchmarking, and presenting a data-driven evidence base to support change.
We’ve seen that age is not a barrier to digital solutions. Clinical buy-in is essential to patient buy-in, and working closely with an experienced technology partner is also vital to successful implementation. Our experience is that RPM has the potential to make significant health improvements and quality of life impacts for patients and releases clinical time.
Ben Matthews, Clinical lead Physiotherapist, Orthopaedic Prehabilitation